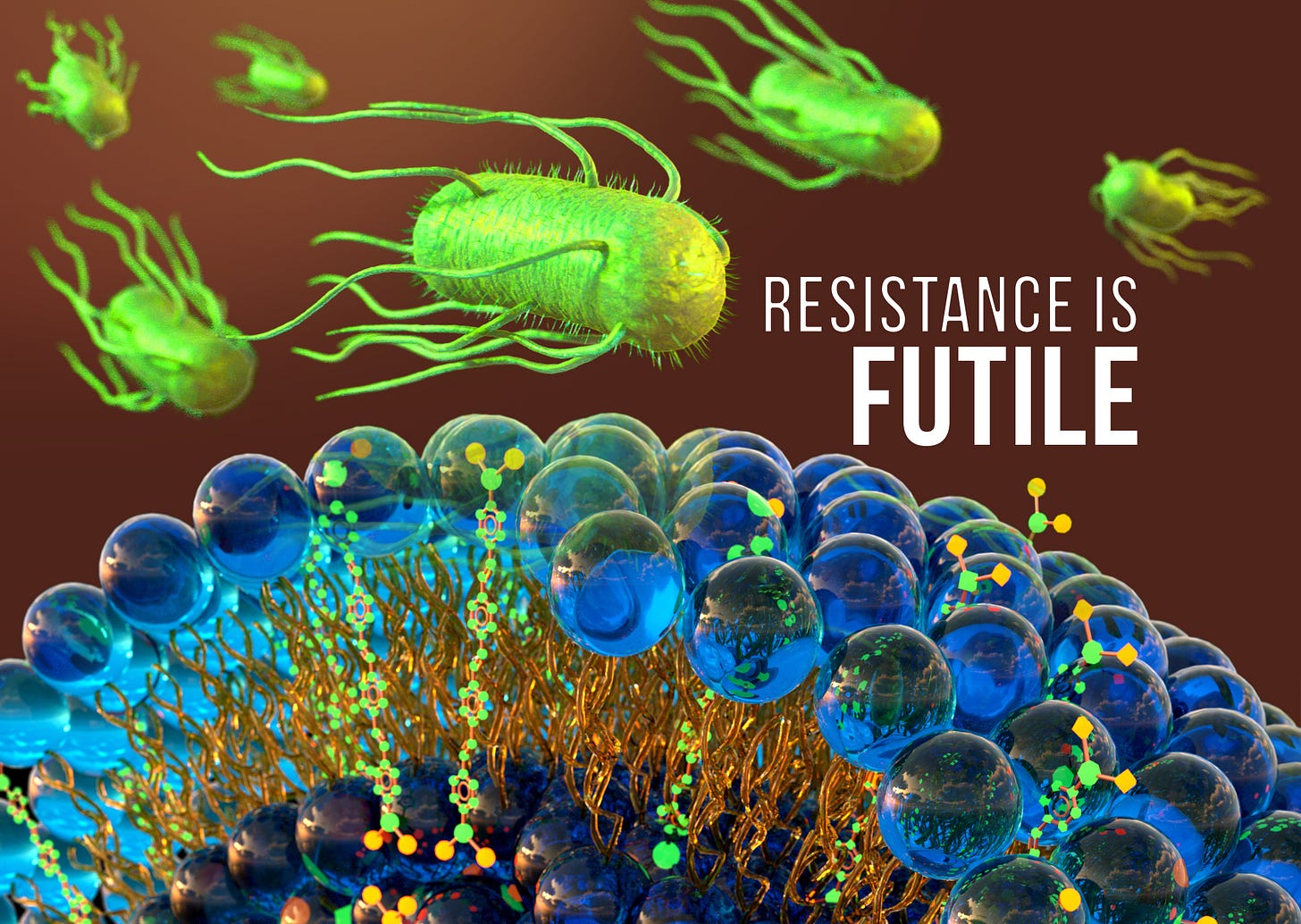
A new antimicrobial cured mice infected with bacteria deemed nearly “untreatable” in humans — and resistance to the drug was virtually undetectable.
The World Health Organization has identified antimicrobial resistance as a major threat to global health. Bacterial resistance to antibiotics only increases over time. The problem is made worse by the fact that the incentives to discover and develop new antibiotics aren’t aligned with the pharmaceutical industry model.
It takes billions of dollars to bring a drug to market and years to recover that investment. Sporadic 10-day prescriptions can’t compete with lifelong prescriptions for blood pressure reduction, cholesterol management etc. in terms of ROI. As a result, only one new class of antibiotic has been developed since the year 2000 and there are few new candidates on the horizon.
In a previous episode, I spoke to Dr. Randy Rohde about methicillin-resistant Staph aureus and the importance of science communication in public health.
In this episode, I talked to Mike Mahan, Professor in the Department of Molecular, Cellular and Developmental Biology at UC Santa Barbara. We talked about:
The challenges of developing new antibiotics and the need for new business models or societal incentives to pay for them
A supplement to the gold standard test for susceptibility that can lead to better patient outcomes
A promising candidate for a new class of broad-spectrum antimicrobial for which resistance is virtually undetectable
Tackling the problem of antibiotic resistance will take effort on multiple fronts. As a society, we need to recognize the seriousness of the problem and decide to invest in the development of new drugs and models that can support that development. For example, a subscription model where companies are paid to develop and have antibiotics on hand whether or not they are used - a kind of strategic reserve. Jason Scharf and I discussed this in a previous episode.
Improved Predictive Susceptibility Test
First of all, are we using the antibiotics we have to our best advantage? Apparently not.
The gold standard test for antibiotic susceptibility is done in rich media (ideal conditions for bacterial growth). If the test more accurately reflected in vivo conditions, would the same results be observed? Mahan and his colleagues have done the test. Comparing the results of the susceptibility test done in either rich or minimal growth media (closer to the host environment) with the ability of an antibiotic to cure sepsis in mice, in ten percent of cases there was disagreement between the gold standard test and the new test in terms of a clinical threshold: Is the bacteria resistant or susceptible?
Using this test, we now check FDA-approved antibiotics that are dismissed by the gold standard test… there were several antibiotics that were highly effective in treating sepsis in mice that are never used by physicians because the gold standard test says it won't work. Consequently, our toolbox for antimicrobial infections is much larger than we once thought.
A promising new class of antimicrobial
In a separate line of inquiry, conjugated oligoelectrolytes (COEs) were being investigated by a colleague for charging cellphones on the battlefield - a bacterial battery if you will, using bacteria and an energy source to drive electron transport. It’s no surprise that pumping electrons out of the cell for this purpose, rather than inward, is harmful to the bacteria in the long run.
Because of this, it was hypothesized that COEs might be candidates as new antibiotics. Mike was skeptical. He thought that these compounds would be comparable to using bleach - great at killing bacteria, and very toxic for humans. “This is gonna be a really short collaboration,” he told his lab manager.
Not subscribed yet? Let’s fix that right here.
Thanks for listening to the podcast and sharing this post.
They tested 17 different COE compounds for antimicrobial activity and toxicity in mammalian cells. All 17 had no problem killing bacteria. And most of them were highly toxic for mammalian cells, as predicted. But one of the 17, COE2-2hexyl, showed promise as being less toxic for mammalian cells.
The next thing they did was immediately test this compound for its effectiveness at curing sepsis in mice. Mice were infected with a range of pathogens, including an isolate from a patient that had succumbed to refractory bacteremia - a multiply-resistant strain of Klebsiella from a community-derived urinary tract infection.
They evaluated toxicity in mice via a blinded measurement of attitude scores (appearance/activity/clinical signs) as an outcome of drug treatment. The compound was well tolerated and able to cure sepsis in mice.
However, the most remarkable observation was that resistance to this compound is virtually undetectable and it is effective against both gram-positive and gram-negative bacteria, presumably because it interferes with multiple membrane-based functions.
Reflecting on this episode, beyond the obvious takeaways here about business models, improved testing and innovation, is the need to allow room for doing some things differently.
I just learned this week that RNA editing is a thing and might be tested as a therapy ( I don’t remember for what) in clinical trials. This is a long way from what I knew about RNA, even in graduate school. But I was not surprised because remarkable innovations pop up every week in our industry.
What is surprising is that a simple innovation that challenges a decades-old susceptibility test is met with resistance (no pun intended) because “that’s the way it’s always been done.” That resistance isn’t really a challenge about the science. It’s one of psychology - getting people to change their habits and ways of thinking.
This has been a summary of the technical highlights. If you want the entertaining story of the scientific journey, give the full episode a listen. I think you’ll enjoy our lively conversation.
Nature Medicine: How to Fight Antibiotic Resistance
Your deepest insights are your best branding. I’d love to help you share them. Chat with me about custom content for your life science brand.















Share this post